Urinary incontinence, the involuntary leakage of urine, is a condition that affects millions of people worldwide. While it is more common in older adults, it can affect people of all ages and genders. Fortunately, with the right treatment and lifestyle adjustments, many can regain control over their bladder and significantly improve their quality of life. This comprehensive guide will explore Urinary Incontinence Treatment, provide expert-backed tips, and offer practical strategies to help you manage and overcome this condition for long-term relief.
What Is Urinary Incontinence?
Urinary incontinence is the inability to control the bladder, leading to unwanted leakage of urine. The severity of the condition can vary, from occasional minor leaks when coughing or sneezing to sudden, strong urges to urinate that are hard to control.
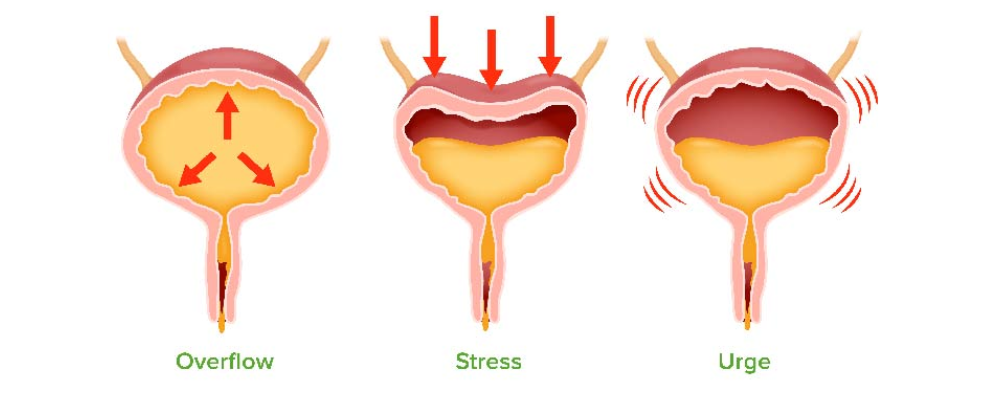
There are several types of urinary incontinence:
- Stress Incontinence: Leakage occurs due to pressure on the bladder from physical activities such as coughing, sneezing, laughing, or exercising.
- Urge Incontinence: A sudden, intense urge to urinate followed by involuntary leakage. This type is often linked to overactive bladder syndrome.
- Overflow Incontinence: When the bladder doesn’t empty completely, causing frequent or constant dribbling.
- Functional Incontinence: Occurs when physical or mental impairment prevents one from reaching the toilet in time.
- Mixed Incontinence: A combination of stress and urge incontinence.
Regardless of the type, there are many treatments available that can help you regain control and improve your overall well-being.

Treatment Options for Urinary Incontinence
Urinary incontinence treatment varies depending on the type and severity of the condition. Below are the most common and effective treatments available:
1. Lifestyle Modifications
One of the simplest and most effective initial steps in managing urinary incontinence is making lifestyle adjustments. Changes in diet, fluid intake, and physical activity can have a significant impact on your symptoms.
- Fluid Management: Regulating your fluid intake can help prevent bladder overfilling, reducing the chances of leakage. Avoid consuming excessive amounts of fluids at one time, and try to drink throughout the day.
- Dietary Changes: Certain foods and beverages can irritate the bladder, making incontinence worse. Limiting caffeine, alcohol, spicy foods, and carbonated drinks can help reduce bladder irritation.
- Weight Management: Obesity puts extra pressure on the bladder, worsening symptoms of stress incontinence. Maintaining a healthy weight can significantly reduce leakage.
2. Pelvic Floor Exercises (Kegels)
Strengthening the pelvic floor muscles through exercises such as Kegels is a cornerstone of incontinence management. These exercises involve tightening and holding the muscles that control urination, which can help improve bladder control.
- How to Perform Kegels: Locate the pelvic muscles by stopping urination mid-stream. Once identified, contract these muscles for 5-10 seconds, then relax for the same amount of time. Repeat this cycle several times a day.
Studies show that consistent practice of pelvic floor exercises can lead to a 70% improvement in incontinence symptoms within 3 to 6 months.
3. Bladder Training
Bladder training involves teaching your bladder to hold urine for longer periods, reducing the frequency of urination and urgency. This method is particularly useful for urge incontinence.
- Scheduled Voiding: Gradually increase the time between bathroom trips, aiming for intervals of 2 to 3 hours.
- Delayed Urination: When the urge strikes, try delaying urination for a few minutes. Over time, this can help extend the time between trips to the bathroom.
4. Medications
Several medications can help control bladder overactivity or strengthen the muscles involved in urination:
- Anticholinergics: These drugs help relax the bladder muscles, preventing spasms that cause urge incontinence. Common examples include oxybutynin and tolterodine.
- Mirabegron: A newer drug that relaxes the bladder, allowing it to hold more urine and reducing the frequency of incontinence episodes.
- Topical Estrogen: For postmenopausal women, topical estrogen applied directly to the vaginal area can help improve bladder function by strengthening the tissues.
5. Medical Devices
For women with stress incontinence, certain medical devices can offer relief by supporting the bladder and urethra.
- Pessaries: A small device inserted into the vagina that helps support the bladder, preventing leakage during physical activities.
- Urethral Inserts: Temporary devices placed in the urethra to block urine leakage during certain activities.
6. Minimally Invasive Procedures
If conservative treatments aren’t effective, there are several minimally invasive procedures available:
- Botox Injections: Botox can be injected into the bladder muscle to reduce overactivity, especially for patients with urge incontinence.
- Nerve Stimulation (Neuromodulation): Electrical stimulation is used to target the nerves controlling the bladder, helping reduce the symptoms of overactive bladder and urge incontinence.
7. Surgery
For severe cases of urinary incontinence that don’t respond to other treatments, surgery may be the best option. Common surgical options include:
- Sling Procedures: A sling is placed around the urethra and bladder neck to provide additional support and prevent leakage.
- Bladder Neck Suspension: This surgery lifts and supports the urethra and bladder neck to reduce stress incontinence.
Expert Opinions on Long-Term Relief
Leading urologists and experts at Advanced Urology and Regeneration emphasize a comprehensive approach to managing urinary incontinence. Dr. Jane Doe, a specialist in urinary health, states:
“A combination of pelvic floor exercises, lifestyle changes, and medical intervention can lead to significant improvements in most patients. The key is early intervention and a customized treatment plan based on the individual’s specific needs.”
Additionally, a 2021 study published in the Journal of Urology highlighted the effectiveness of combining bladder training with medications, showing up to a 50% reduction in symptoms for patients who adhered to the plan for over 6 months.
What Foods Stop Urination?
Diet plays a significant role in managing urinary incontinence. While certain foods and drinks can worsen bladder control, others can help reduce the frequency and urgency of urination.
- Bananas: High in potassium, bananas can help regulate fluid balance in the body and reduce urinary urgency.
- Whole Grains: Foods high in fiber, such as oats and brown rice, can help prevent constipation, which can worsen urinary incontinence.
- Lean Proteins: Chicken, turkey, and fish provide essential nutrients without irritating the bladder, unlike spicy or acidic foods.
- Non-citrus Fruits: Fruits like apples and berries are good choices, as they do not irritate the bladder like acidic fruits (e.g., oranges and lemons).
- Water-rich Vegetables: Cucumbers and celery, though rich in water, can help flush toxins from the body without overstimulating the bladder.
Advanced Urology and Regeneration: Your Trusted Partner in Urinary Incontinence Treatment
At Advanced Urology and Regeneration, we understand the profound impact that urinary incontinence can have on your daily life. Our clinic offers cutting-edge treatments tailored to your unique needs, combining the latest medical advances with personalized care. Our team of specialists is committed to providing you with the most effective solutions for managing urinary incontinence, helping you regain control, confidence, and comfort.
Whether you are seeking minimally invasive procedures, medication, or expert advice on lifestyle changes, Advanced Urology and Regeneration is here to guide you every step of the way. Contact us today to learn more about our comprehensive approach to Urinary Incontinence Treatment.
Conclusion
Urinary incontinence is a manageable condition with a wide range of treatments available. From lifestyle changes and pelvic floor exercises to medical interventions and surgery, there are options to suit every need. At Advanced Urology and Regeneration, we are committed to helping you regain control and improve your quality of life.
If you or a loved one is struggling with urinary incontinence, don’t hesitate to reach out to our experts for personalized advice and effective treatment plans.

